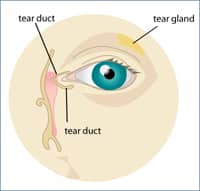
 The eye’s tear ducts, also called the nasolacrimal ducts, are small tubes that stretch from the eye into the nose. They are responsible for carrying tears away from the eyes into the nasal cavity, where they naturally are absorbed or eventually swallowed. An obstructed tear duct can be caused by a wide range of problems, such as excessive tearing and chronic eye infections. It can be present at birth or acquired through infection, inflammation or eye diseases. In some cases, an obstructed tear duct can also be age-related or a result of a physical injury to the eye.
The eye’s tear ducts, also called the nasolacrimal ducts, are small tubes that stretch from the eye into the nose. They are responsible for carrying tears away from the eyes into the nasal cavity, where they naturally are absorbed or eventually swallowed. An obstructed tear duct can be caused by a wide range of problems, such as excessive tearing and chronic eye infections. It can be present at birth or acquired through infection, inflammation or eye diseases. In some cases, an obstructed tear duct can also be age-related or a result of a physical injury to the eye.
Takle Eye Group is proud to have Leiv M. Takle Jr. MD providing various orbital disorder treatments for our patients.
Types of Tear Duct Disorders
Congenital nasolacrimal duct obstruction is blockage of a tear duct that has failed to open properly at birth. It occurs in about 6 percent of infants and is characterized by persistent watery eyes or a discolored discharge. Although most cases of congenital nasolacrimal duct obstruction resolve with time, some may lead to infections and other complications. Takle Eye Group are staffed with qualified specialists who can help.
Acquired nasolacrimal duct obstruction is blockage of a tear duct that typically develops in adulthood. There are two types of the disorder: primary and secondary. Primary acquired duct obstruction occurs for no apparent reason, and the cause is often unknown. Secondary acquired duct obstruction is often the result of an acute underlying eye condition such as a cyst, tumor, inflammation, physical injury or nasal and sinus disease.
Dacryocystitis is an acute infection of the nasolacrimal sac that is generally caused by a nasolacrimal duct obstruction. It is associated with swelling, pain and redness, and when left untreated may lead to eye infections and even corneal ulceration.
Punctal stenosis occurs when the puncta (small openings along the eyelid margin through which the tears drain) are abnormally narrow. This usually leads to excessive tearing and secondary blurred vision. Successful treatment is often achieved with medicated eye drops or a minor office procedure to enlarge the tear duct openings.
Lacrimal gland and lacrimal sac tumors are rare and complex medical conditions that can be life-threatening when not promptly diagnosed and treated. Several different types of tumors can affect the eye’s tear gland, and some are more serious than others. Tear duct tumors can spread and affect several structures of the eye and, in some cases, may lead to severe facial deformities. Routine eye exams are essential in identifying lacrimal gland and sac tumors.
Treatment Options
Takle Eye Group is staffed with talented surgeons who provide comprehensive, multidisciplinary care to our middle Georgia eye care patients who suffer from tear duct disorders. We utilize the latest, most advanced medical and surgical treatments to help you overcome conditions that may jeopardize your eye health and impair your vision. Regular and complete eye exams are key to protecting your eyes from tear duct disorders.
To schedule your routine eye exam or learn more about your treatment options at Takle Eye Group please contact us today at 770-228-3836 to make an appointment.
Eye Socket Disorders
Thyroid Eye Disease
Patients who have thyroid disease, either too high functioning or too low functioning, can develop significant changes in the appearance and comfort of their eyes. These changes include greater prominence of the eyes, noticeable puffiness of the eyelids or significant discomfort in their eyes.
A small number of patients with thyroid disease can develop sudden and severe changes in the eye socket that leads to compression of the optic nerve and secondary loss of vision. Patients who are newly diagnosed with thyroid disease or those with known thyroid disease but a new change in the appearance of their eyes or their vision, should see an ophthalmic plastic surgeon for further evaluation and recommendations for monitoring and treatment for their eye condition.
Enucleations/Prosthesis
Enucleation refers to the surgical removal of an eye. Enucleation is usually performed for several different reason:
- to remove a malignant tumor that has developed within the eye
- to alleviate intolerable pain in a blind eye affected by a condition such as uncontrollable glaucoma
- to reduce the risk of “sympathetic ophthalmic”
- severe inflammation of unknown cause which may affect the remaining eye when one eye has been severely injured and blinded.
Removal of an eye is considered a drastic and traumatic measure to most people. Although many patients who require this surgery have no vision in the affected eye, those who do have vision recognize that enucleation will result in instantaneous, permanent, total blindness of that eye. Furthermore, all patients who undergo this procedure will require an artificial eye (ocular prosthesis) as a cosmetic substitute for the real eye.
Surgical Procedure
Enucleation is usually performed under general anesthesia, although it can be done under local anesthesia by numbing the entire eye and socket tissues prior to the surgery. The procedure generally takes no more than 60 minutes.
Immediately after the eyeball has been removed, an orbital implant, only slightly smaller than the eye, is inserted deep in the socket. The implant is covered externally with the pink surface tissue that lines the eyelids and the ultimate result is a surface that is similar to the inner lining of the mouth.
Postoperative Care
At the completion of the enucleation, a pressure patch is applied over the eyelids. This patch is intended to keep swelling of the socket tissues to a minimum. It is generally kept in place for about one to four days after surgery. During the time this patch is in place, the patient commonly experiences some difficulty opening the lids of the unoperated eye. This can be quite frightening to the patient.
Fortunately, the difficulty in opening the eyelids generally resolves itself after the first post-operative day. Moderate post-surgical pain in the socket generally occurs during the first 24 hours, but pain relievers are usually prescribed as needed to reduce this discomfort. After the pressure patch is removed, the eyelids are usually swollen and black-and blue for a few days. The use of ice compresses on the eyelids generally helps to reduce the swelling rapidly. Ointment which promotes healing of the socket tissues are usually started as soon as the pressure patch has been removed.
Ocular Prostheses
The cosmetic artificial eye (ocular prosthesis) is a plastic device that is molded to fit between the eyelids over the conjunctiva that covers the ball implant. This prosthesis is generally made three to six weeks after enucleation, in order to allow the socket tissues time to heal adequately. Prior to that time, a thin clear plastic plate (conformer) is usually worn in place of the prosthesis. This conformer helps to prevent shrinkage of the space between the inner surface of the lids and the mucus membrane covering of the ball implant. Until the ocular prosthesis is fitted, the upper eyelid may be droopy. The eyelid droop usually resolved in several weeks or months, but may occasionally require surgery to lift the eyelid. In some cases, the ocular prosthesis supports the eyelid and generally allows the lids to open and close normally.
Some tearing of the eye is normal once the prosthesis is in place. In some patients, thick mucus may build up on the prosthesis requiring that the artificial eye be removed and washed off from time to time. In most instances, mucous buildup can be washed off the prosthesis and out of the socket by using an irrigation solution without removing the prosthesis. However, most patients remove their prosthesis for cleaning once every on to three months.